Urethritis, Infection vs. Chemical (Adult Female)
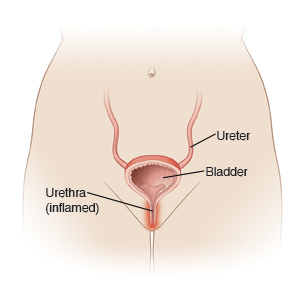
You have urethritis. This means there is swelling (inflammation) in your urethra. The urethra is the tube that drains the urine out of your bladder. Urethritis is most often caused by a bacterial infection. This may be from gonorrhea, chlamydia, or another sexually transmitted infection (STI). Other causes of urethritis may include irritation from soap, lotion, deodorant, or spermicides. Hormone changes that happen after menopause may also cause it. The cause of your urethritis is not known.
Women with urethritis often don't have symptoms. When symptoms do happen, they can be the same as a urinary tract infection or bladder infection. Symptoms can include:
-
Burning or pain when urinating
-
Feeling like you have to urinate often
-
Pus coming from your vagina
-
Pressure or pain in your lower belly (abdomen)
-
Pain when you have sex
Urethritis caused by bacteria is treated with antibiotics. It may clear up in a few weeks or months, even without treatment. But if you don't get treatment, the bacteria that cause the infection can stay in the urethra. Even if symptoms go away, you can still have the infection. And you can spread it to others.
Your sex partner or partners may also need to be treated. This is true even if they have no symptoms. You can get infected again if they aren't treated and you have sex with them. Your partner should call their healthcare provider to be examined and treated if needed.
Home care
Follow these guidelines when caring for yourself at home:
-
Stop using anything that may cause irritation. This includes soap, lotions, or other chemicals.
-
If you were given antibiotics, take them until they are all gone unless your healthcare provider tells you to stop. It's important to finish the antibiotics even if your symptoms go away. This is to make sure the infection has completely cleared up.
-
Don't have sex until both you and your partner have finished all the antibiotics and your provider tells you that you can't pass on the infection.
-
You can take acetaminophen or ibuprofen for pain, unless you were given a different pain medicine to use. If you have long-term (chronic) liver or kidney disease, talk with your provider before taking these medicines. Also talk with your provider if you've had a stomach ulcer or gastrointestinal bleeding, or are taking blood- thinner medicines.
-
Learn about safe sex practices and use them. The safest sex is with a partner who does not have an STI and has sex only with you. Condoms may keep you from getting some STIs. These include gonorrhea, chlamydia, and HIV. But condoms are not a guarantee you won't get these diseases.
Follow-up care
Follow up with your healthcare provider, or as advised. If an STI culture was taken, call as directed for the result. If you are diagnosed with an STI, follow up with your provider or your local health department. You should have a complete STI screening, including HIV testing. For more information, call CDC-INFO at 800-232-4636.
When to get medical advice
Call your healthcare provider or get care right away if any of these occur:
-
You don't get better after 3 days
-
Fever of 100.4ºF (38ºC) or higher, or as directed by your provider
-
New pain in your lower belly or back
-
Pain in your lower belly or back that gets worse
-
Repeated vomiting
-
Vaginal discharge or unexpected vaginal bleeding
-
Weakness, dizziness, or fainting
-
You can't urinate because of the pain
-
Rash or joint pain
-
Painful open sores on the outer vaginal area
-
Enlarged, painful lumps (lymph nodes) in your groin